Understanding tooth abscess stages is crucial – it determines whether you can save your tooth or if it requires extraction. If you’re experiencing sudden tooth pain, swelling, or a pimple-like bump on your gums, identifying the stage of your infection helps you get the right treatment quickly.
This guide explains what happens at each stage of a tooth abscess, what symptoms to watch for, and why timing matters for your overall health.

The 4 Stages of a Tooth Abscess In a Nutshell:
- Stage 1: Enamel Decay & Initial Infection – Bacteria attack the outer tooth layer through plaque buildup or a crack. You may notice tooth sensitivity to hot and cold, or slight discomfort when chewing. This stage can progress silently over weeks or months if untreated.
- Stage 2: Dentin & Pulp Inflammation – Infection spreads deeper into the softer layers beneath the enamel. Pain becomes sharper and more noticeable, often described as throbbing or dull aching. At this point, a cavity is typically visible, and root canal treatment may save the tooth.
- Stage 3: Abscess Formation – Pus collects at the tooth’s root, creating a pocket of infection. Symptoms escalate to intense, constant pain (especially when lying down), facial swelling, difficulty chewing, and sometimes a visible “pimple” on the gums. This stage demands urgent dental care.
- Stage 4: Advanced Infection (Emergency) – If left untreated, the abscess spreads beyond the tooth root to the surrounding bone and tissues. You may experience fever, swollen lymph nodes, difficulty swallowing, or facial swelling. Infection can enter the bloodstream, causing serious health risks. Immediate professional intervention is critical.
Firstly, let’s look at what a tooth abscess is;
What is a Tooth Abscess?
A dental abscess develops when bacteria gain access to the inside of your tooth or the surrounding gum tissue, triggering your body’s immune response to fight the infection. The result is a painful pocket of pus – essentially your body’s natural defence mechanism working overtime.
The culprits are usually preventable: untreated cavities, advanced gum disease without intervention, or a cracked or knocked-out tooth that creates a pathway for bacteria. What many patients don’t realise is that an abscess is a warning sign that your tooth is in serious trouble. We’ve helped countless patients save teeth at this stage with root canal treatment and expert care. Left unaddressed, however, an abscess can escalate from a painful nuisance to a genuine health emergency.
Now, let’s take a look at each stage of a tooth abscess in a little more detail so you can understand what might be causing your pain and what you can do about it.

Stage 1: Enamel Decay & Initial Infection
What Happens at This Stage
Plaque (a sticky film of bacteria) builds up on your teeth. If not removed through brushing and flossing, the bacteria produce acids that attack tooth enamel, your tooth’s protective outer layer. A small cavity forms as the enamel breaks down. At this point, the infection hasn’t reached deeper layers, and your tooth’s pulp (the nerve centre) remains unharmed. This is why Stage 1 is the most treatable: a simple tooth filling stops progression entirely.
Symptoms to Notice
Many people have no symptoms at Stage 1, which is why it often goes undetected. When symptoms appear, they’re mild: slight tooth sensitivity to hot, cold, or sweet foods; minor discomfort when chewing; or a barely noticeable ache. Some patients report a visible white spot or a small dark hole on the tooth surface. Because these signs are easy to dismiss, regular dental checkups are essential – your dentist can spot decay before you feel pain.
Timeline
Stage 1 typically develops over weeks to months, depending on your oral hygiene and diet. If you catch it early through routine checkups, treatment is quick and straightforward. However, if ignored, the infection progresses to Stage 2 within weeks. This is why we emphasise preventive care: addressing decay at this stage prevents months of pain and costly treatment later on down the line.
Stage 2: Dentin & Pulp Involvement
Progression of Infection
The cavity deepens as bacteria penetrate the dentin layer (the softer tissue beneath enamel). The infection continues towards the pulp chamber, where your tooth’s nerve and blood vessels sit. As bacteria invade the pulp, it becomes inflamed and irritated. At this stage, antibiotics won’t stop the infection; you need professional intervention. Root canal treatment becomes the primary option to save your tooth.
Pain Escalation
Pain shifts from mild sensitivity to persistent, noticeable discomfort. You may experience sharp, throbbing pain, especially when eating, drinking hot or cold beverages, or lying down (pressure changes intensify the ache). Some patients describe it as constant dull pain punctuated by sharp spikes. The pain often radiates to your jaw, ear, or neck. Sleep disruption is common. At this stage, over-the-counter painkillers provide temporary relief but won’t address the underlying infection.
Why Delay is Risky
Waiting at Stage 2 allows bacteria to destroy more of your tooth’s interior structure. The longer the infection sits in the pulp, the greater the risk it spreads beyond the tooth root into the jawbone and surrounding tissues. This progression moves you into Stage 3 – where treatment becomes more complex, painful, and expensive. Early intervention at this stage through root canal treatment typically saves your natural tooth.
Stage 3: Abscess Formation
Pus Pocket Development
At tooth abscess stage 3, the infection has now created a collection of pus at the tooth’s root. This abscess is your body’s attempt to wall off the infection and prevent it from spreading further. However, the pressure from this pus buildup is what causes the intense pain. The abscess may remain contained at the root tip (periapical abscess) or form between the tooth and gum (periodontal abscess). Either way, the pocket won’t drain on its own and requires professional treatment to resolve. This is when we typically recommend urgent root canal therapy or, if the tooth is beyond saving, extraction.
Visible Signs & Symptoms
Pain reaches a new level at stage 3 – often described as unbearable, constant throbbing that worsens when you lie down or bite down. Swelling appears in your face, jaw, or neck as the infection triggers an inflammatory response. You may notice a small, pimple-like bump on your gums (this is the abscess attempting to drain). Bad breath and a foul taste in your mouth are common, along with difficulty chewing, swallowing, or difficulty opening your mouth fully. Some patients develop a low-grade fever. At this stage, ignoring the problem is no longer an option.
Urgency Level
This is an urgent situation. You should contact your dentist immediately – ideally on the same day symptoms appear. If it’s after hours, call our emergency line; we offer 24-hour support because Stage 3 infections can escalate quickly. Do not delay, hoping the pain subsides. Do not rely on antibiotics alone – they may reduce symptoms temporarily but they won’t eliminate the tooth abscess. Professional drainage or root canal treatment is essential. The longer you wait, the higher the risk of spreading to your jawbone and beyond.
Stage 4: Advanced Infection (Emergency)
Complications That Can Occur
If Stage 3 goes untreated, the infection breaks through the confines of your tooth and spreads into the surrounding bone, deeper jaw tissues, and potentially your bloodstream. Bone infection can develop, causing permanent damage to the structures supporting your teeth. In rare but serious cases, the infection can trigger Ludwig’s angina – a deep space neck infection that can obstruct your airway and become life-threatening. The abscess may also spread to your sinuses, causing chronic sinus problems. At this advanced stage, tooth extraction becomes unavoidable, and you’ll need aggressive antibiotic therapy alongside professional drainage to prevent systemic complications.
Systemic Symptoms
Stage 4 symptoms extend beyond your mouth. You may experience high fever (often above 38°C), severe chills, and generally feel unwell throughout your body. Swollen lymph nodes in your neck become pronounced and tender. Difficulty swallowing or speaking increases significantly. Some patients report difficulty breathing or a “stiff neck” sensation. Facial or neck swelling can become dramatic. These are signs the infection is affecting your entire body, not just your tooth. This stage demands emergency medical and dental intervention – do not self-treat or wait for an appointment.
When Immediate Care is Non-Negotiable
Go to an emergency room or call emergency services if you experience:
- High fever combined with facial/neck swelling
- Difficulty breathing or swallowing
- Confusion or disorientation
- Severe swelling that restricts your airway
- Signs of sepsis (rapid heartbeat, dizziness, extreme fatigue)
Call Pure Dental immediately (24 hours) if you have:
- Intense, unbearable tooth pain with visible swelling
- Pus drainage from your gum
- Swelling spreading across your face or jaw
- Fever under 38°C with obvious abscess symptoms
At Stage 4, every hour counts. This is a medical emergency that could have serious consequences if left unaddressed. Our emergency dentists are equipped to drain the abscess, prescribe antibiotics, and prevent life-threatening spread.
What are the Different Types of Tooth Abscesses?
Types of dental abscesses include:
Periapical Abscess (Most Common)
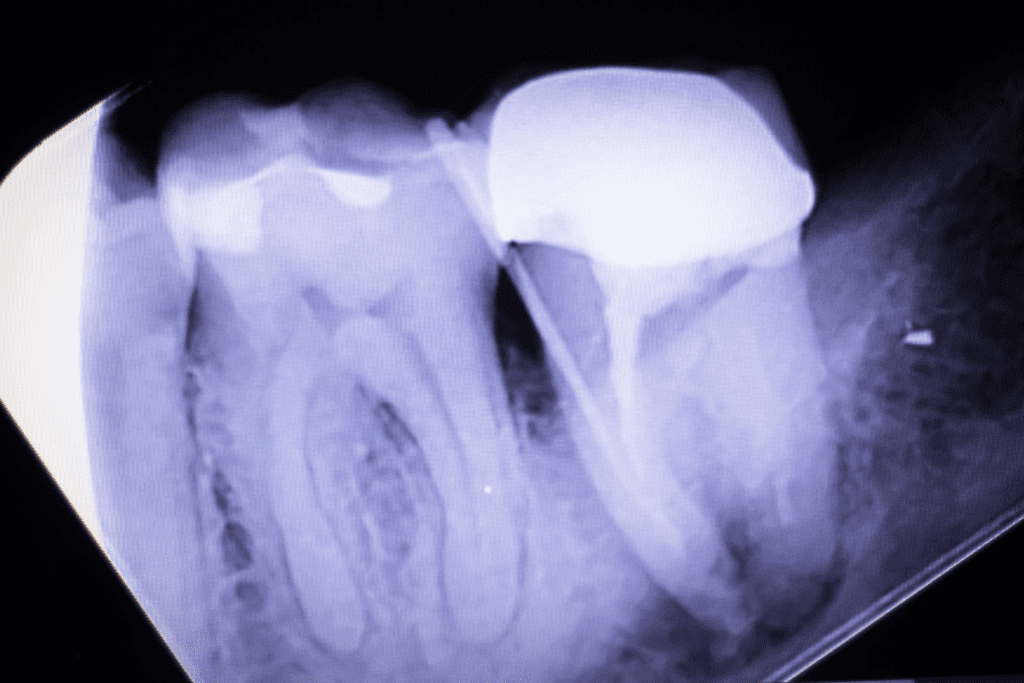
This is the abscess type you’ve likely read about in the earlier tooth abscess stages. It forms at the tip of the tooth’s root after infection spreads deep into the pulp. The abscess sits in the bone directly beneath your tooth, which is why you experience intense throbbing pain and facial swelling. It’s the most common type because it develops from the inside out, making early detection difficult. At Pure Dental, we typically address periapical abscesses with root canal treatment. The good news: if caught at Stages 2-3, we can save your natural tooth through endodontic therapy. Waiting until Stage 4 often means extraction becomes necessary.
Periodontal Abscess
This abscess forms in the gum tissue itself, usually in the pocket between your tooth and gum – often triggered by advanced gum disease (periodontitis) or a traumatic injury to the area. Unlike periapical abscesses that develop from within the tooth, periodontal abscesses form from the outside in. You may notice swelling and tenderness in the gum, along with pus drainage. It’s particularly dangerous because the pus can easily spread deeper into the gum tissue and bone without obvious early warning signs. Treatment involves professional cleaning of the gum pocket, drainage if necessary, and sometimes antibiotic therapy. Regular gum health checks are essential for prevention – this is why we emphasise the importance of professional cleanings and early gum disease treatment.
Gingival Abscess
A gingival abscess is the least serious type, forming only on the surface of your gum tissue (usually appearing as a small, pimple-like bump). It typically results from food or a foreign object becoming trapped between your teeth and gum, or occasionally from a minor injury to the gum. Unlike the other types of abscesses, it doesn’t involve your tooth’s root or deep bone structures, so it’s usually easier to treat and resolve. However, it remains uncomfortable and can become infected if left untreated. A simple professional hygienist cleaning to remove trapped debris and allow drainage often resolves the issue. If symptoms persist, we may prescribe antibiotics or recommend gum therapy. The key difference: gingival abscesses rarely threaten tooth loss, but they’re still a sign you need professional care to prevent complications.

Early Warning Signs: Don’t Miss These
Subtle Symptoms You Might Ignore
The earliest signs are often so mild you might dismiss them. You may notice slight discomfort when biting down on one tooth, or a dull ache that comes and goes. Your tooth might feel slightly raised or loose.
Some patients report a faint bad taste or minor gum redness around one tooth. You assume it needs better flossing or that the pain will pass. These quiet symptoms are your tooth’s first cry for help.
Early detection is when a routine checkup becomes invaluable – we catch tooth decay before pain forces you to act.
Red Flag Symptoms (Stage 3)
Now the signs are unmistakable. Sharp, throbbing pain keeps you awake. Your face or jaw shows visible swelling. You notice a pimple-like bump on your gum, possibly with drainage. Don’t try managing this with painkillers alone. Call us immediately – this is urgent but not yet life-threatening. We can often save your tooth if you act now.
Emergency Symptoms That Demand Same-Day Care (Stage 4)
You’re running a fever (38°C or higher) with severe facial or neck swelling. You’re struggling to swallow or speak. Breathing feels restricted. You feel systemically unwell: severe fatigue, rapid heartbeat, or confusion. Swelling is spreading across multiple areas of your face and neck (and sometimes even to other parts of the body). This isn’t something to manage from home. Call emergency services or go to A&E immediately. Notify us so we can coordinate your care.

Can You Treat a Tooth Abscess at Home?
Why Home Remedies Don’t Work
Salt water rinses, essential oils, turmeric paste – they feel like you’re doing something, but they won’t eliminate an abscess. Here’s why: an abscess is already formed deep inside your tooth or gum tissue. Topical treatments can’t reach it.
Pus won’t drain with home remedies. The bacteria won’t die without professional intervention. You might get temporary pain relief, which feels like progress, but the infection spreads underneath. Oral antibiotics can slow bacterial growth and stop the infection from spreading, but they can’t eliminate a formed abscess. Only professional drainage, root canal treatment, or extraction removes the source. Home remedies won’t stop what’s already happening inside.
What You Can Do for Temporary Relief
While waiting for your appointment (ideally same-day), manage pain temporarily. Take paracetamol or ibuprofen as directed. Apply a cold compress to your cheek for 15 minutes at a time. Sleep with your head elevated – lying flat increases pressure and pain. Use these measures for short-term comfort, not as treatment. Get professional care scheduled.
Why Professional Treatment for a Tooth Abscess is Essential
Only a dentist can stop the infection at its source. We remove infected tissue through root canal therapy, drain the abscess, or extract the tooth if necessary. We prescribe antibiotics that address your specific infection. We have the expertise to prevent spread to your jawbone, sinuses, or bloodstream.
At Pure Dental, we assess the severity of the tooth abscess and its stages, explain options clearly, and act promptly. The golden rule is, don’t gamble with an abscess!

Prevention: Stop the Abscess Before It Starts
Daily Oral Hygiene Habits
- Brush twice daily with fluoride toothpaste, spending at least two minutes on all surfaces. Don’t just rush through it – focus on the gum line where plaque builds up. Floss every single day. This removes bacteria and food debris where your toothbrush can’t reach.
- Consider using an electric toothbrush if you struggle with the manual brushing technique. Rinse with water after meals if you can’t brush. Avoid sugary snacks between meals – they feed the bacteria that cause decay.
Good oral hygiene is your first line of defence. It stops decay before it starts, which means no cavities, no infection, no abscess.
Regular Checkups & Early Detection
Visit Pure Dental every six months for a routine checkup and clean. We spot early decay, gum disease, and other issues before they become problems. Caught early, a small cavity costs far less than root canal treatment later.
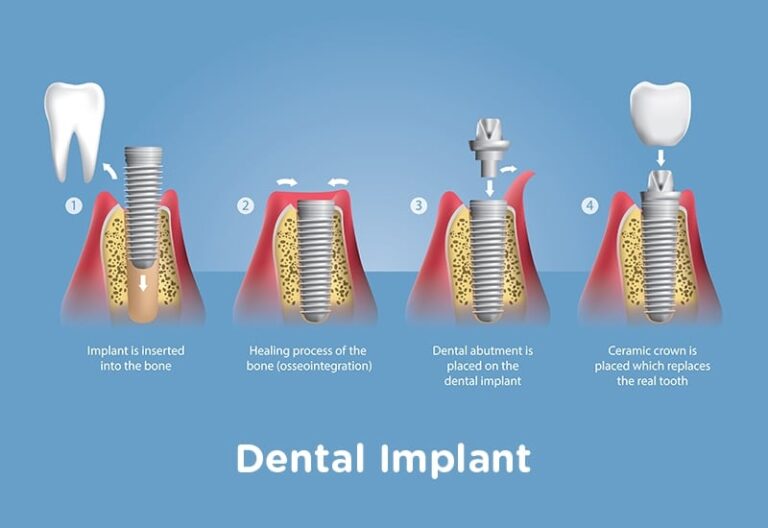
X-rays help us see decay between teeth and below the gum line. Professional cleaning removes tartar buildup that brushing can’t eliminate. We also screen for gum disease, which is a major abscess risk.
Many patients who develop abscesses haven’t had a checkup in years. Don’t be that person. Regular visits literally prevent emergencies.
Foods & Habits to Avoid
- Limit sugary drinks and snacks – bacteria thrive on sugar.
- Don’t use your teeth as tools to open packages or crack ice. Avoid chewing on hard objects like pen caps.
- If you play contact sports, wear a mouthguard to prevent tooth trauma.
- Don’t smoke -it weakens your immune system’s ability to fight infection and damages gum health.
- If you grind your teeth at night, talk to us about a nightguard.
These small habit changes significantly reduce your risk of abscess. Protect your teeth as you would any valuable investment.
Why Preventive Care Beats Emergency Treatment
A routine checkup costs far less than emergency root canal treatment or extraction. Prevention saves money, time, and pain.
You keep your natural teeth – nothing replaces them perfectly. You avoid the complications that can arise from an untreated infection. Most importantly, you stay healthy. Systemic infections from abscesses can affect your heart, kidneys, and overall well-being.
Think of prevention as insurance. A small investment now stops you from paying a much larger price later.
Experiencing Tooth Pain? Get Expert Care Today
Don’t ignore tooth discomfort. Even mild sensitivity or a slight ache deserves professional attention – it could be the earliest warning sign of an abscess developing.
Pure Dental offers same-day emergency appointments because we know dental pain can’t wait. Our endodontics-trained dentists use advanced microscope technology to save teeth that others might recommend extracting. We’re open 24 hours and ready to help.
Whether you’re experiencing early warning signs or full-blown emergency symptoms of a dental abscess, we’re here to stop the infection and protect your tooth.
Call us 24hrs on 01872 222 404
Don’t wait for an abscess to become unbearable. Contact Pure Dental today – because when it comes to tooth pain, early action saves your smile.
Tooth Abscess Stages FAQs
Q: How long does a tooth abscess take to develop?
It depends on the cause. A cavity-related abscess typically develops over weeks to months if untreated. A tooth abscess from trauma or infection can form in days. Once it reaches Stage 3, progression accelerates quickly. This is why early detection matters – catching it early stops the clock.
Q: What does a tooth abscess look like?
You might see a small, pimple-like bump on your gum near the affected tooth. The area around it may appear red and swollen. The bump might drain, leaving a foul taste. Your tooth could look discoloured or appear slightly loose. Not all abscesses are visible on the surface, which is why imaging and professional examination are important.
Q: Can antibiotics cure a tooth abscess?
No. Antibiotics slow bacterial growth and may temporarily reduce symptoms, but they can’t eliminate an established abscess. Only professional drainage, root canal treatment, or extraction removes the source of infection. Antibiotics are prescribed alongside professional treatment to prevent spread, not as a standalone cure.
Q: Will my tooth abscess go away on its own?
Absolutely not. An abscess won’t resolve naturally. It may rupture and drain temporarily, giving you false relief, but the infection remains. Without treatment, it continues spreading into your bone and bloodstream. Ignoring an abscess and hoping it will heal itself is a serious mistake.
Q: Is a tooth abscess an emergency?
It depends on the stage. Stage 3 (visible swelling, intense pain) requires urgent same-day care. Stage 4 (fever, difficulty swallowing, facial swelling) is a medical emergency – go to A&E or call 999. Even Stage 2 pain deserves urgent attention. If you’re in doubt, call us here at Pure Dental in Truro. We offer 24-hour support.
Q: What’s the difference between a pimple and an abscess on the gums?
A pimple is typically a surface skin issue unrelated to your teeth. A gum abscess is always connected to a tooth or gum infection and won’t resolve without professional treatment. An abscess may look similar to a pimple, but it’s painful, firm, and doesn’t pop like a normal pimple. If you’re unsure, we can examine it
Q: How do I know if my tooth abscess is severe?
Severe abscesses may present with fever, widespread facial swelling, difficulty swallowing or breathing, and systemic symptoms such as fatigue or a rapid heartbeat. Even without these, an abscess is always serious because it will progress if untreated. Don’t wait for it to become severe – any abscess needs professional care.
Q: How to tell if an abscess is getting worse?
Watch for increasing pain despite painkillers, spreading swelling to your face or neck, fever development, or difficulty eating and speaking. If symptoms worsen rapidly, the abscess is spreading. This is when you need emergency care – don’t wait for the next available appointment.
Q: How long does it take for a dental abscess to spread?
It varies. Some abscesses spread slowly over weeks; others escalate dramatically within days. Once it reaches your jawbone or bloodstream, the spread accelerates significantly. This unpredictability is why we stress urgency – don’t give the infection time to spread.
Q: Can you get an abscess on your wisdom teeth?
Absolutely. Wisdom teeth are prone to decay and gum disease because they’re hard to clean. An abscess here can be particularly painful and dangerous because of its proximity to deeper facial spaces. If you have wisdom tooth pain, contact us immediately.
Q: Can a tooth infection cause eye twitching?
It’s uncommon, but yes. Severe infections can cause nerve irritation that affects surrounding areas, including facial nerves. If you’re experiencing eye twitching alongside tooth pain, this is a sign that the infection is significant. Seek professional care promptly.
Q: How to treat a gum abscess in a child?
Don’t delay. Contact your dentist or paediatric dentist immediately. Children’s infections can spread faster due to their developing immune systems. Treatment depends on the abscess type and severity – professional examination is essential. Avoid home remedies; get professional care.
Q: Can a tooth abscess cause neck pain?
Yes. An abscess at the tooth’s root can cause pain that radiates to your jaw, ear, and neck – sometimes making you think the problem is elsewhere. If you have tooth pain with neck discomfort, the abscess may be more advanced. This combination warrants urgent dental evaluation.